How it works:
Share your skin goals and snap selfies
Your dermatology provider prescribes your formula
Apply nightly for happy, healthy skin
How it works:
How it works:
Share your skin goals and snap selfies
Your dermatology provider prescribes your formula
Apply nightly for happy, healthy skin
How it works:
Skincare 101: What is acne anyway?
Think you’re breaking out? Here's your one-stop acne guide from the experts.

In this article
Acne can be incredibly frustrating to deal with. The good thing is, that there are steps you can take to reduce it and to help prevent it from occurring. The thing is, everyone’s skin is unique—so there’s no one-size-fits-all solution to this skin condition. That’s why we’ve put together this starter guide to help you identify what kind of breakouts you might be having and your options for treatment. If you’re new to skincare, congratulations on taking your first steps on your journey to clear skin! At Curology, we believe that knowledge is power when it comes to taking care of your skin.
What is acne?
Acne is a common skin condition that appears when hair follicles clog with oil (sebum) from the sebaceous glands and dead skin cells. Bacteria that normally live on the skin thrive in the excess oil, an inflammatory response occurs, and acne is formed!¹ Types of acne include blackheads, whiteheads, papules, pustules, and cystic acne. Millions of people experience it every year, so chances are you have or have had acne or someone you know currently has or has had acne. Nothing to be ashamed about!
As common as it may be, treating acne can be challenging because the skin is complex. Your skin is a microbiome, home to fungus and bacteria that can lead to breakouts and skin inflammation when things are off-balance.
What are the symptoms of acne?
If you’re wondering how to identify if you have acne, there are a few symptoms you can look for.² Common acne symptoms can include:
Inflamed red bumps, also called papules
Pus-filled bumps with a red ring around the perimeter also called pustules
Small white bumps, called whiteheads (aka closed comedones)
Small black bumps, called blackheads (aka open comedones)
Deep bumps that can be sensitive to the touch, possibly cysts or nodules
The causes of acne
Acne is multifactorial—that’s dermatologist-speak for having multiple, intersecting contributing factors. Genetics can play a role, and so can hormonal changes.³ The causes of acne can be different for each person because, again, everyone’s skin is unique (something we think is to be celebrated!). Once you understand the symptoms and different types of acne, the next step in treating your breakouts and preventing future ones is identifying potential contributing factors:
Genetics
Hormones
Lifestyle
Environmental triggers
Pore-clogging ingredients in makeup, hair, and skincare products
Skin inflammation
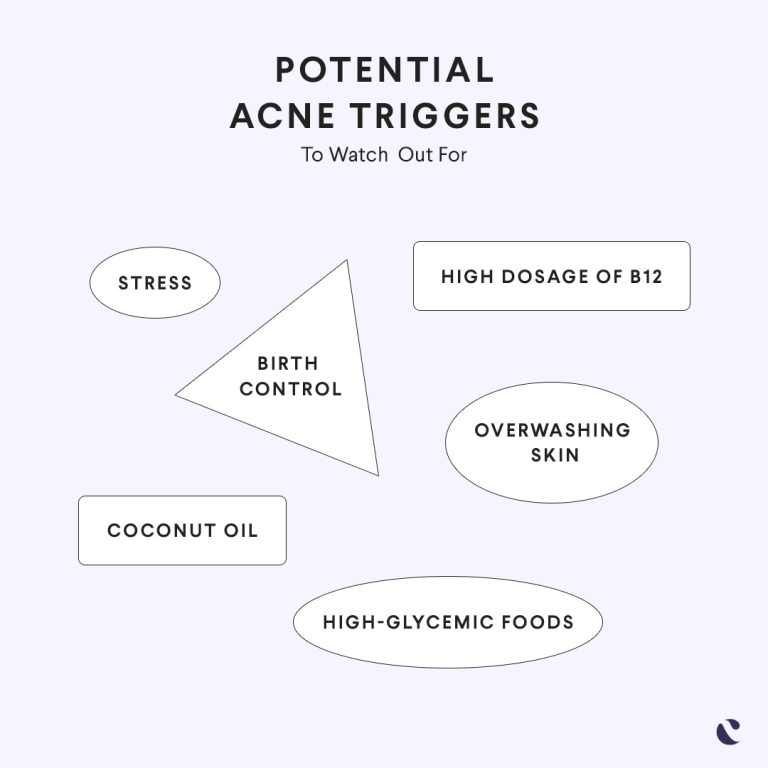
Lifestyle and other causes of acne
In addition to having acne-prone skin, several other environmental and lifestyle factors can contribute to breakouts. The good news? Once you know what kinds of factors may trigger your acne, you can take steps to reduce their impact.
Diet. Evidence suggests certain foods can trigger acne in some people,⁴ while others might help you to achieve better skin.⁵
Stress. Stress can indirectly trigger breakouts because our bodies respond to pressure by releasing certain hormones, and these hormones may lead to acne.⁶
Workouts. Working out is good for your health (and your skin), but sweat and friction may also lead to breakouts.⁷
Pillowcases. Just like sweaty workout clothes, pillowcases can harbor product residue, moisture, and other acne triggers.
You can also unintentionally trigger breakouts by touching your face with your hand or your phone or by using products with potentially pore-clogging (aka comedogenic) ingredients. Living a completely acne-free lifestyle may seem difficult or even impossible. But just by being aware of these triggers, you can do your best to avoid them.
How does acne form?
To understand how acne forms, it’s important to know how pores become clogged. If the natural skin cell renewal process gets thrown off, the build-up of dead skin cells and sebum (aka the oil skin naturally produces) can lead to clogged pores and breakouts. Acne treatments that stabilize your skin cell turnover and help shed dead skin cells are generally effective at eliminating and helping to prevent clogged pores.
So—what creates the inflammation we often see with acne? We know that our skin is a natural microbiome where microorganisms like bacteria and fungi live. One type of bacteria, Cutibacterium acnes (or C. acnes), can irritate the skin when it feeds off excess oil in a clogged pore. The inflammatory response to the overgrowth of bacteria is what we know to be acne.
What are the different types of acne?
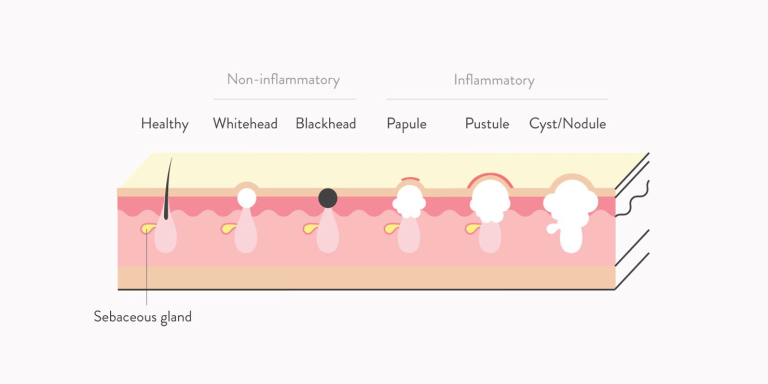
With so many causes of breakouts, it’s no surprise that there are also many different types of acne. Chances are, your breakouts can be described as one or more of the following:⁸
Whiteheads: Small clogged pores that look like a small white bump because of trapped oil and dead skin cells
Blackheads: Small clogged pores that turn black because the trapped oil and dead skin cells are exposed to the air
Fungal acne: Small, uniform bumps that tend to spread across a central area—especially on the forehead, jaw, chest, or back
Papules: Tender bumps with redness and swelling caused by inflammation, usually less than 5 millimeters in size
Pustules: Large, inflamed pimples that might look like a big whitehead
Nodules: Large, firm, reddish lumps without pus that extend deeper than a papule and are often painful
Cysts: Large, soft, under-the-skin pimples that go deep under the skin’s surface and may feel swollen and tender
Who can get acne?
Contrary to popular belief, teenagers aren’t the only ones who can suffer from acne. Adults do, too—especially women! One study found that almost half of women in their 20s and a quarter of women in their 30s experience acne.⁹ Also, nearly 20% of newborns up to 6 weeks old, infants, and small children may also develop acne.¹⁰
How to treat acne
We know acne is complicated—and it’s not always easy to get rid of. Typically, the best way to treat acne is to take a simple approach. You’ll want to maintain a minimalist skincare routine tailored to your specific skin needs while also avoiding things that can make acne worse. You have many options when it comes to acne treatment, from topical creams to oral medications.

How to treat hormonal acne
Breaking out with hormonal acne is frustrating—especially if you’re dealing with other hormone-related symptoms. Certain hormonal fluctuations—starting a new birth control, pregnancy, hormonal therapy, or even your period (to name a few)—can cause glands in your skin to release more oil (aka sebum), which can collect in the pores and contribute to acne. To treat or help prevent hormonal acne, you may have to reevaluate your diet, reduce stress, or even directly address your hormones. Here are some treatment options for hormonal acne:
Spironolactone is a pill you can take to reduce your levels of acne-causing hormones.¹¹
Birth control pills can potentially help acne if they have the right combination of hormones,¹² but talk to your medical provider first.
Spearmint tea. Drinking two cups of spearmint tea per day may help reduce acne-causing androgens.¹³
You’ll also want a gentle, no-clog skincare routine that makes sense for the specific kind of breakout you’re having. A licensed medical provider with training in skincare (like the experts at Curology) can help you come up with a custom treatment plan that’s tailored just for you.
How to treat blackheads
One of the best strategies for treating comedones like blackheads and whiteheads includes skincare products (both prescription and over-the-counter) that help unclog pores:
Tretinoin is a topical prescription treatment that helps normalize the lifecycle of skin cells, helping to reduce blocked pores.¹⁴
Azelaic acid works to unblock pores and helps reduce post-inflammatory hyperpigmentation.¹⁵
Salicylic acid is a beta-hydroxy acid (BHA) that chemically exfoliates the skin, helping to clear out pores.
How to treat fungal acne
If your breakouts are uniform, itchy bumps, you may have fungal acne. Fungal acne is caused by pityrosporum, a type of fungus that naturally lives on the skin. In addition to eliminating potential fungal acne triggers like dirty, sweaty pillowcases, look for acne treatments with these ingredients:
Zinc pyrithione has antimicrobial properties that help to stop the growth of the fungus that can lead to fungal acne.¹⁶
Azelaic acid has antimicrobial and anti-inflammatory properties that treat acne by keeping acne-causing bacteria and fungus in check.
Ketoconazole treats fungal acne by killing microorganisms that can fuel breakouts, while its anti-inflammatory effects help soothe the skin.¹⁷
While these ingredients are available over-the-counter, more potent varieties of all three are also available with a prescription from your medical provider.
How to treat cystic acne
Cystic acne is generally deeper, more swollen, stubborn to resolve, and can even be painful. Cysts generally heal on their own, but it can take time. If you’d like help in speeding up the process, here are some treatments for cystic acne:
Spot patches (or hydrocolloid bandages) can be a good option for a cyst. They can speed healing while shrinking the cyst through the absorption of pus and oil.
A warm compress can help reduce swelling. A steeped-and-cooled bag of green tea is a great compress that may also reduce redness.
Cortisone injections will help dissolve a cyst quickly. You can get one from in-person healthcare professional.¹⁸
Don’t try to pop your cyst. Attempting to pick, squeeze, or pop a cystic pimple isn’t something you want to do! First of all, it probably won’t work—it’s too deep beneath the skin. Secondly, messing with it can worsen the inflammation and the pain.¹⁹
What are some potential complications of acne?
Ideally, once acne heals, it leaves no evidence that it was ever there in the first place. But it’s important to know that in some cases, acne can result in scarring and discoloration.
Scarring. Scarring can occur especially as a result of inflammatory acne. One of the best ways to help prevent acne scars is by not popping or picking at pimples.
Post-inflammatory hyperpigmentation. Hyperpigmentation can follow damage to the skin, including acne lesions. Hyperpigmentation appears as discoloration of the skin but does not affect the texture of the skin, unlike acne scars.²⁰
Post-inflammatory erythema. This occurs when a pink or red discoloration remains after an acne lesion heals.²¹
Helping prevent acne
To keep it simple, let’s start with basic tips to make sure you don’t accidentally make acne worse or trigger new breakouts:
Try not to overdo it. Be gentle and patient—your skin needs time to heal. Avoid harsh scrubbing, over-exfoliation, and risky at-home hacks.
Don’t pop. Even though it’s instant gratification, popping is likely to slow down your healing process and can potentially lead to scarring.²²
Avoid hot water. Lukewarm water is best for most skin types (you can damage your skin with burning hot water). Cold water is fine, too, but it’s a myth that it shrinks your pores.
Eat mindfully. Sugar, dairy, and certain carbs can contribute to breakouts in some people.²³ Keep this in mind when planning meals.
Check your ingredients. Avoid skincare products that contain ingredients that can potentially make acne worse. Skip face wash with sodium lauryl sulfate (SLS) and moisturizers with cocoa butter, along with these other ingredients. Look for skincare and haircare products labeled non-comedogenic to avoid clogging your pores.
Use acne treatments. A great step to help prevent acne is to consistently use over-the-counter acne treatments such as benzoyl peroxide or salicylic acid. Remember to apply the treatment to all areas that you tend to break out or use as directed by your medical provider.
Do laundry more often. Remember, pillowcases, athletic clothes, and other fabrics that repeatedly come into contact with skin may contribute to breakouts.
How severe can acne get?
Acne ranges from mild to very severe. Currently, there’s no official ranking system for determining the severity of acne, but taking inventory—specifically, knowing the types of blemishes and an approximate idea of how many you have—can be a great help in determining an effective treatment plan.
According to one study that ranked the severity of acne based on the number of acne lesions,²⁴ people with zero to five blemishes were considered to have mild acne, six to 20 were moderate, 21-50 were severe, and more than 50 blemishes were very severe.
Another study looked at the different types of blemishes to determine the severity of acne.²⁵ Acne consisting of some comedones (whiteheads and blackheads) was considered mild. Some comedones and few papules and pustules meant mild to moderate. Some papules and mustules and many comedones meant moderate. Many papules and pustules were considered moderate to less severe. Many papules and pustules along with nodules constituted severe acne.
What to do when your acne won’t clear
For some people, washing your face daily, using a good moisturizer, and avoiding products with pore-clogging and irritating ingredients are enough to clear up acne. For others, simple yet effective acne treatment can help. If over-the-counter isn’t cutting it, it may be time to talk to a dermatology provider about prescription acne treatments. Reach out to the skin experts at Curology and start your customized acne treatment plan for free.
Curology’s dermatology providers are here for you
Curology’s medical providers are board-certified doctors, licensed physician assistants, and nurse practitioners who’ve completed specialized training in treating acne in all skin. So when you’re a Curology member, it’s about more than just skincare products—it’s about getting expert guidance on your journey to clear skin.
Get your personalized skincare routine with Curology
Get your personalized skincare routine with Curology

Acne can be frustrating, which is why Curology creates personalized, dermatology-backed skincare made for you. Curology can help you find the right acne treatment for you by using the right ingredients to target your specific acne. You won’t only receive effective acne treatments for your skin, but you’ll get guidance from dermatology providers to answer your questions, too.
Sign up for a 30-day free trial for just $4.95 + tax (to cover shipping and handling).
FAQs
Acne is a common skin condition that appears when hair follicles clog with oil (sebum) from the sebaceous glands and dead skin cells. Bacterial that normally lives on the skin thrives in the excess oil, an inflammatory response occurs, and acne is formed!
Common acne symptoms can include:
Inflamed red bumps, also called papules
Pus-filled bumps with a red ring around the perimeter also called pustules
Small white bumps, called whiteheads (aka closed comedones)
Small black bumps, called blackheads (aka open comedones)
Deep bumps that can be sensitive to the touch, possibly cysts or nodules
Typically, the best way to treat acne is to take a simple approach. You’ll want to maintain a minimalist skincare routine tailored to your specific skin needs while also avoiding things that can make acne worse. You have many options when it comes to acne treatment, from topical creams to oral medications.
Scarring. One of the best ways to help prevent acne scars is by not popping pimples.
Post-inflammatory hyperpigmentation. Appears as discoloration of the skin but does not affect the texture of the skin, unlike acne scars.
Post-inflammatory erythema. Pink or red discoloration remains after an acne lesion heals.
If over-the-counter isn’t cutting it, it may be time to talk to a dermatology provider about prescription acne treatments. Reach out to the skin experts at Curology and start your customized acne treatment plan for free.
P.S. We did the research so you don’t have to:
Toyoda, M., & Morohashi, M. Pathogenesis of acne. Medical electron microscopy: official journal of the Clinical Electron Microscopy Society of Japan. (2001).
Cleveland Clinic. Acne. (2020, September 1).
Zaenglein, A. L., et al.Guidelines of care for the management of acne vulgaris. Journal of the American Academy of Dermatology. (2016 February 17).
Zaenglein, A. L., et al.Guidelines of care for the management of acne vulgaris. Journal of the American Academy of Dermatology. (2016 February 17).
Mahmood, S.N., et al., Diet and Acne Update: Carbohydrates Emerge as the Main Culprit. Journal of Drugs in Dermatology. (2014, April).
American Academy of Dermatology.Adult Acne. (n.d.).
Mill. O. H. Acne Mechanica. (April 1975).
Cleveland Clinic. Acne. Ibid.
Perkins, A. C., et al. Acne vulgaris in women: prevalence across the life span. Journal of women's health. ( February 2012).
American Academy of Dermatology. Is that acne on my baby's face? (n.d.).
Zaenglein, A. L., et al.Guidelines of care for the management of acne vulgaris. Ibid.
Zaenglein, A. L., et al.Guidelines of care for the management of acne vulgaris. Ibid.
Grant P.Spearmint herbal tea has significant anti-androgen effects in polycystic ovarian syndrome. A randomized controlled trial. Phytotherapy research. ( February 2010).
Baldwin, H. E., et al.40 years of topical tretinoin use in review. Journal of drugs in dermatology. ( June 2013).
Zaenglein, A. L., et al.Guidelines of care for the management of acne vulgaris. Ibid.
Gupta, M., et al.Zinc therapy in dermatology: a review. Dermatology research and practice. (2014, July 10).
Anwar, A., & Kamran Ul Hassan, S.Two Percentage of Ketoconazole Cream for the Treatment of Adult Female Acne: A Placebo-Controlled Trial. Cureus. (2020, November 19).
Mayo Clinic.Acne. (n.d.).
American Academy of Dermatology. Pimple popping: why only a dermatologist should do it. (n.d.).
Silpa-Archa, N., et al. Postinflammatory hyperpigmentation: A comprehensive overview: Epidemiology, pathogenesis, clinical presentation, and noninvasive assessment technique. Journal of the American Academy of Dermatology. (2017).
Bae-Harboe, Y. S., & Graber, E. M. Easy as PIE (Postinflammatory Erythema). The Journal of clinical and aesthetic dermatology. (September 2013).
American Academy of Dermatology. Pimple popping: why only a dermatologist should do it.Ibid.
Zaenglein, A. L., et al.Guidelines of care for the management of acne vulgaris. Ibid.
Hayashi, Nobukazu et al. Establishment of grading criteria for acne severity.The Journal of dermatology (May 2008).
Bernardis, Elena et al. Development and Initial Validation of a Multidimensional Acne Global Grading System Integrating Primary Lesions and Secondary Changes. JAMA dermatology. (2020 March1)
This article was originally published on October 21, 2020, and updated on July 14, 2022.
*Cancel anytime. Subject to consultation. Results may vary.
Curology Team

Nicole Hangsterfer, PA-C
Related Articles
Does dermaplaning cause acne? Experts explainThe 6 best chemical exfoliators for glowing skinNavigating the world of oil-free moisturizers: Our top 4 picksHow long does a rosacea flare-up last? Experts explainPeptides for skin: Unpacking their skincare influencePopular Articles
Ask Curology: Is my cold breaking me out?Slugging: The dermatologist-approved skincare hack going viral on TikTokTretinoin vs retinol: What’s the difference?How to create a self-care routine that actually sticksYour 2023 skincare horoscopeTry prescription skincare
Get routine essentials

Good skin days ahead
- Breakouts
- Redness
- Fine lines
- Dark spots
- Hair thinning